Now, the same group of biomedical pioneers have taken the next step in advancing a platform to allow reanimation of paralyzed limbs under direct control of the brain.
The upgraded system, called ReHAB (for “Reconnecting the Hand and Arm to the Brain”), uses an array of several sensors surgically implanted into different brain areas along with high-density stimulating electrodes placed directly on hand, arm, and shoulder nerves. The researchers work with the new system to give paralyzed people the ability to do more than ever before. A clinical trial is underway to evaluate its safety and effectiveness.
“WITH REHAB, WE are IMPLANTING A SOPHISTICATED SYSTEM THAT LETs THE BRAIN MOVE THE ARM IN NATURAL WAYS USING THOUGHT ALONE, SOMETHING THAT HAS NEVER BEEN DONE BEFORE.”
Jonathan Miller, MD, former Professor of Neurosurgery at UH and Case Western Reserve School of Medicine
Dr. Sweet is joined by co-principal investigators Bolu Ajiboye, PhD, Associate Professor of Biomedical Engineering at Case Western Reserve University (CWRU), Emily Graczyk, PhD, Assistant Professor of Biomedical Engineering at CWRU, and Robert Kirsch, PhD, Professor and Chair of Biomedical Engineering at CWRU and Executive Director of the Cleveland Functional Electrical Stimulation (FES) Center.
Funded by a $3 million grant from the United States Department of Defense and supported by U.S. Food and Drug Administration investigational device approval, the new system allows participants to control the movement of their own hand and arm by thinking about those movements. The system also offers participants a chance to regain sensation in the hand.
But there could be more: Ajiboye said researchers hope to restore to clinical trial participants something called “proprioception”—the ability to know where your limb is even with your eyes closed.
“We aim to restore different sensory perceptions, including touch and proprioception, to persons with paralysis by applying electrical micro-stimulation directly to the brain,” Ajiboye said. “Not only will doing so likely enhance the restored motor function, but we believe the level of ownership felt by participants will also be significantly increased. Direct sensory feedback will enhance the feeling that ‘This is mine, my arm. This is me.’”



Kirsch said the leap from BrainGate to ReHAB is on two fronts—the brain interface and the functional electrical stimulation (FES)—but that in both cases it has required a committed collaboration.
“This is not just a demo this time, but a way to give real function to these folks,” he said. “But these kind of projects really are what I would call big, team science, and it takes all of us to make this happen.”
How ReHAB works
ReHAB has several new and different features compared with other systems, according to Dr. Miller.
“ReHAB is different from previous work in the area in several ways,” said Dr. Miller. “For the first time, we are simultaneously looking at several different brain areas involved in movement planning. In addition, we are using new peripheral nerve electrodes that were initially designed by Dustin Tyler, PhD (the Kent H. Smith Professor of Biomedical Engineering, Case Western Reserve University, and Associate Director, Cleveland Advanced Platform Technology), to provide stimulation to sensory nerves so that amputees could better use prosthetic arms.
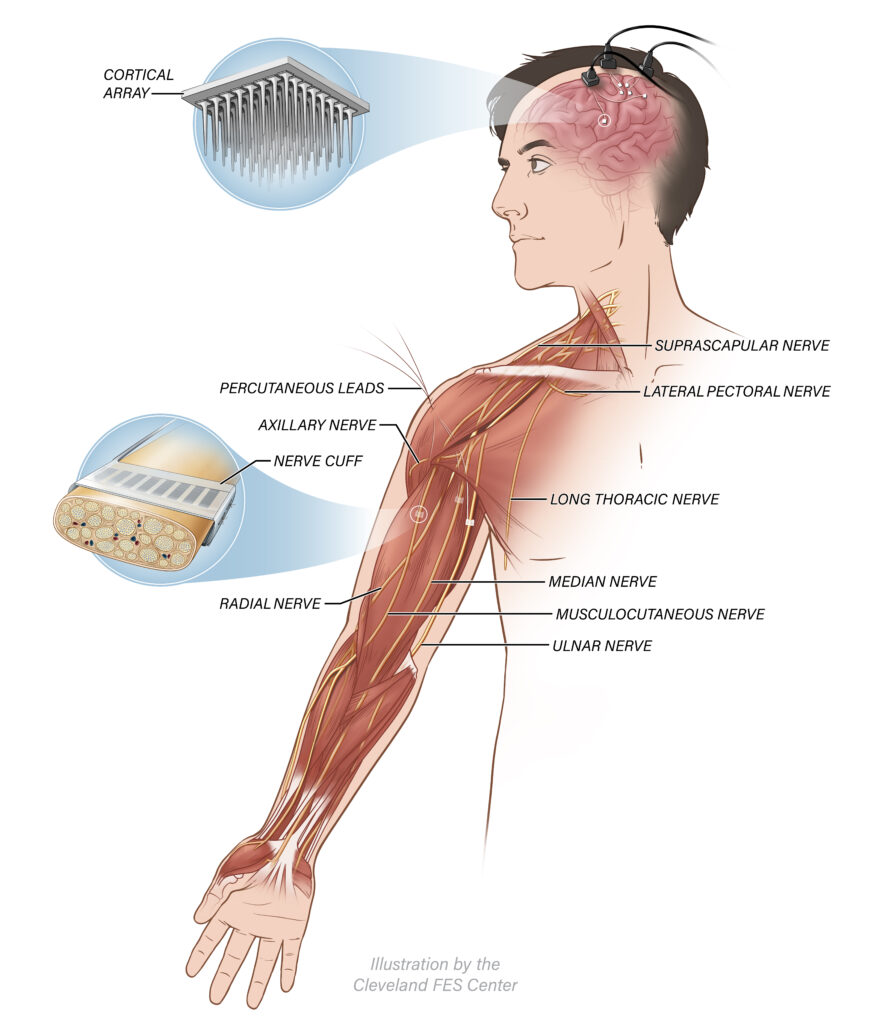
“These electrodes spread the nerve and use many small contacts that are able to stimulate nerve fibers selectively. These electrodes provide even more precise control of movement than we were able to accomplish in our previous studies.”
The nerve electrodes are controlled by signals recorded from several small electric arrays, each about the size of a baby aspirin tablet, implanted into the surface of the participant’s brain to record neural activity related to intended movements. In other words, the brain arrays read the participant’s electrical signals and translate them into command signals used by the peripheral electrodes to control movements of the arms, hands, and fingers.
“Each brain array will have a few-dozen channels and will allow recording from the brain and also stimulation to simulate sensation for feedback,” Dr. Miller said. “The idea is that the patient will not only be able to move his or her hands, but will also be able to tell what the hand is doing, by feeling sensations in the hand and fingers and perceiving where the hand is located.
“It could be a huge step forward to allow paralyzed people to interact with their environment again and regain function lost as a result of disease or injury.”
The brain array is connected by a cable through the skull to amplifiers at the top of the head. The amplifiers are plugged into the arm stimulator to stimulate the muscles.
Cleveland has a long history in FES, with work in upper arm, leg, and trunk stimulation.
Funding Supporters
Department of Defense, Congressionally Directed Medical Research Programs (CDMRP), Spinal Cord Injury Research Program (SCIRP)
US Department of Veterans Affairs, Office of Research and Development
Partners



Latest news and updates
60 Minutes
60 Minutes Overtime – Following the Breakthroughs in Prosthetics
Further video on prosthetics research which includes the ReHAB study
60 Minutes
60 Minutes: “The Feeling of Feeling”
60 Minutes piece about restoring sensation to people with amputations or spinal cord injuries
New York Times